Gingivitis is a prevalent form of gum disease characterized by inflammation of the gingiva, the part of the gum around the base of the teeth. Due to poor oral hygiene, gingivitis manifests as red, swollen gums that may bleed easily, especially during brushing or flossing. Despite being mild and reversible in its early stages, untreated gingivitis can progress to more severe periodontal diseases.
Delving into this query requires us to explore the intricate web of oral health and its potential ramifications for interpersonal relationships.
Pathophysiology of Gingivitis
A grasp of its pathophysiology is crucial to comprehend the contagious nature of gingivitis. The intricate dance between bacteria and our oral environment lays the foundation for this inflammatory condition.
Gingivitis begins with the accumulation of dental plaque, a biofilm teeming with bacteria. When this plaque is not adequately removed, it hardens into tartar, allowing bacteria to thrive and increase. The immune response triggered by the presence of these bacteria leads to the hallmark inflammation and swelling of the gingiva, thus initiating the pathophysiological cascade of gingivitis.
Causes and Risk Factors
Various factors contribute to the development of gingivitis, including smoking, hormonal changes, certain medications, and systemic diseases such as diabetes. Poor nutrition and compromised immune function also elevate the risk of developing gingivitis.
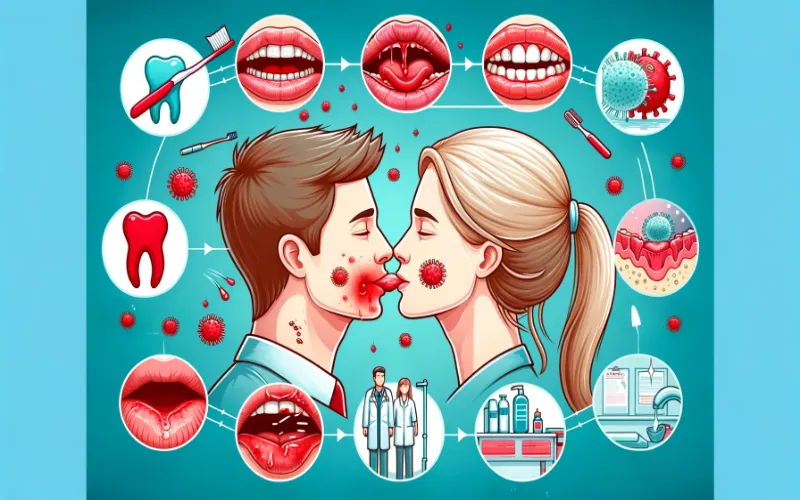
Transmission of Gingivitis
While gingivitis is not contagious, the bacteria responsible for it can be transmitted between individuals. This bacterial exchange often occurs through saliva, meaning activities such as kissing, sharing utensils, or even close personal contact can potentially spread the bacteria that cause gingivitis.
However, it’s important to note that simply having the bacteria does not guarantee one will develop gingivitis. The recipient’s oral hygiene practices and immune response play significant roles in whether or not the bacteria lead to gum inflammation.
So, answering the question “is gingivitis contagious?”.
Yes, gingivitis is not directly contagious, but the bacteria that cause it can be transmitted through close contact. Poor oral hygiene, shared utensils, and intimate activities can facilitate bacterial transfer. Maintaining good oral health practices is essential to prevent the spread of gingivitis within communities.
Symptoms and Diagnosis
Recognizing the signs of gingivitis is pivotal.
- Understanding these symptoms, from subtle changes in gum color to the notorious bleeding during brushing, is our first defense against their progression.
- Swollen, tender gums that bleed easily are often the initial indicators.
- Additionally, gums may recede, creating pockets between the teeth and gums where more plaque can accumulate.
- Persistent bad breath, or halitosis, is another common symptom, often overlooked but indicative of underlying gingival inflammation.
Diagnosing gingivitis typically involves a dental examination. The dentist checks for signs of gum inflammation, measures pocket depths around the teeth, and may use dental X-rays to assess bone loss. Early detection is crucial for reversing the condition and preventing further complications.
Prevention and Personal Health
Maintaining excellent oral hygiene is paramount in preventing the onset of gingivitis.

- Regular brushing with fluoride toothpaste, daily flossing, and an antiseptic mouthwash can significantly reduce bacterial load.
- Routine dental check-ups and professional cleanings are essential in managing plaque and tartar buildup.
- For those with existing symptoms, early intervention through professional cleaning and enhanced home care routines can halt the progression of the disease.
- Additionally, lifestyle changes such as quitting smoking and improving dietary habits can bolster oral health, reducing the risk of gingivitis and its potential transmission.
Factors Influencing Contagion
Although gingivitis is not contagious, several factors influence its development and spread of the bacteria that cause it. The following factors affect the contagion dynamics of gingivitis, revealing the complex interplay between various elements in oral health.
- Frequency of Brushing: The regularity of brushing sessions significantly influences gingivitis contagion, as consistent plaque removal is a primary defense against bacterial proliferation.
- Precision in Flossing: The meticulousness with which individuals engage in flossing directly impacts contagion risks, addressing the areas between teeth that brushing may not effectively reach.
- Quality of Oral Care Products: The choice of toothpaste, mouthwash, and dental tools can affect the efficacy of oral hygiene practices, thereby influencing the potential for gingivitis transmission.
- Immunodeficiency Conditions: Individuals with compromised immune systems face an elevated risk of gingivitis contagion, as their ability to combat bacterial threats is inherently weakened.
- Inflammatory Response Regulation: Understanding how the immune system regulates inflammatory responses to oral bacteria provides insights into its role in either mitigating or exacerbating the contagion risk associated with gingivitis.
- Nutritional Support for Immunity: Adequate nutrition supports a robust immune system, and deficiencies in essential nutrients may compromise the body’s defense against gingivitis, affecting contagion susceptibility.
Controlling the Spread
Maintaining oral health is not solely an individual responsibility; it is essential in curtailing the spread of gingivitis within communities. Empowering individuals with effective preventive strategies is paramount to achieving this goal.
- Professional Cleanings: Dental hygienists play a crucial role in controlling contagion through thorough cleanings. Removing plaque and tartar reduces the bacterial load, preventing the progression of gingivitis.
- Targeted Interventions: In cases of advanced gingivitis, targeted interventions such as scaling and root planing may be necessary. Dental professionals can employ specialized techniques to address the root causes and mitigate contagion risks.
- Education and Counseling: Dental professionals serve as educators, guiding patients on effective oral care practices. Counseling on lifestyle choices and habits further reinforces the importance of personal responsibility in preventing gingivitis transmission.
Conclusion
Whether gingivitis is contagious is answered in a nuanced exploration of factors and preventive measures. As the complexities surround this common dental ailment, a synthesis of personal responsibility and professional intervention emerges as the linchpin in controlling its spread.

Dr. Orion Johnson is a dedicated and compassionate dentist committed to providing exceptional dental care to his patients.Dr. Johnson obtained his Doctor of Dental Surgery (DDS) degree from a prestigious dental school, where he excelled academically and clinically. He is licensed to practice dentistry and stays updated with the technology through continuing education and training.