Gingivitis is a common and often mild periodontal disease characterized by gum inflammation. This condition arises due to the accumulation of plaque, a sticky film of bacteria that constantly forms on teeth. If not removed through regular brushing and flossing, plaque can harden into tartar, leading to gingivitis. While gingivitis is non-destructive in its initial stages, if left untreated, it can progress to more severe forms of periodontal disease.
Understanding Halitosis
Halitosis, commonly known as bad breath, affects a significant portion of the population. It can be caused by various factors, including poor oral hygiene, certain foods, medical conditions, and habits such as smoking. The unpleasant odor originates from the mouth, and in many cases, it is linked to the presence of bacteria.
These bacteria produce sulfur compounds, often responsible for the malodor associated with bad breath. Additionally, conditions such as dry mouth (xerostomia), which reduces saliva production, can exacerbate halitosis. Saliva helps cleanse the mouth by washing away food particles and bacteria. These particles and bacteria can remain in the mouth without sufficient saliva, contributing to bad breath.
Does Gingivitis Cause Bad Breath?
Yes, gingivitis can cause bad breath. Gingivitis is an inflammation of the gums, often caused by plaque buildup. This inflammation can release sulfur compounds and bacteria that contribute to bad breath, also known as halitosis. Maintaining good oral hygiene, including regular brushing, flossing, and dental check-ups, can help prevent gingivitis and reduce the risk of bad breath.
The Pathophysiology of Gingivitis
The pathophysiology of gingivitis involves a complex interaction between bacterial biofilms and the host’s immune response. When plaque accumulates on the teeth and is not adequately removed, it provides a conducive environment for bacteria to thrive. The body’s immune system reacts to these bacteria, leading to inflammation.
The gums become red and swollen and may bleed easily. This inflammatory response is the body’s attempt to fight off the bacterial invasion but also results in the symptoms associated with gingivitis.
Furthermore, if gingivitis is left untreated, chronic inflammation can lead to the destruction of the periodontal ligament and alveolar bone, which support the teeth, potentially resulting in tooth loss and more severe periodontal diseases.
How Gingivitis Contributes to Bad Breath
Gingivitis contributes to bad breath primarily through the activity of bacteria present in plaque. These bacteria produce volatile sulfur compounds (VSCs) as metabolic byproducts responsible for the foul odor. Additionally, the inflamed and bleeding gums create an environment that allows further bacterial growth and the accumulation of food particles, which can exacerbate bad breath.
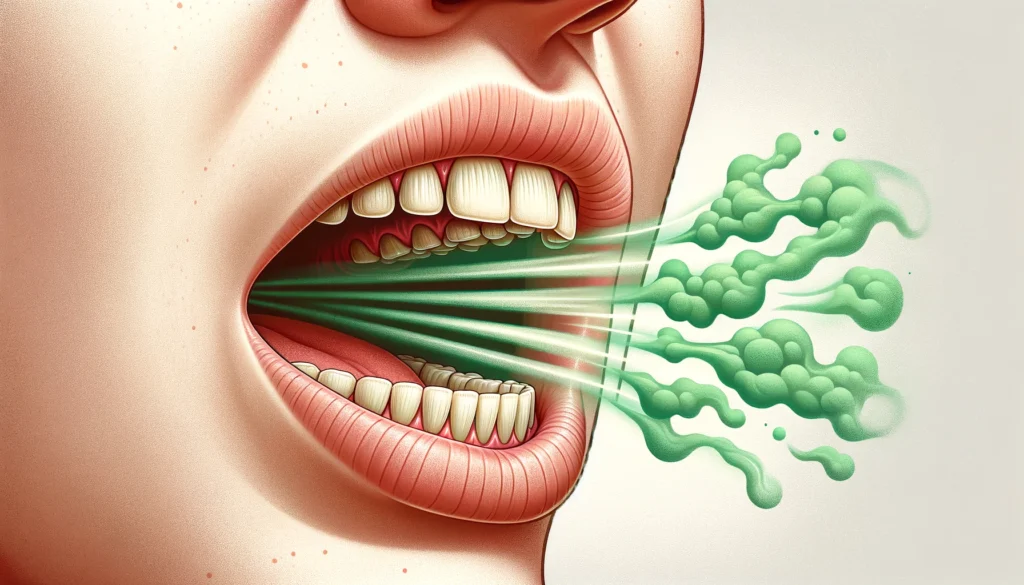
The combination of these factors makes gingivitis a significant contributor to halitosis. Moreover, the constant inflammation and bleeding in the gums provide a source of proteins that bacteria can break down, further increasing the production of malodorous compounds. This cycle underscores the importance of treating gingivitis promptly to maintain oral health and fresh breath.
Symptoms and Diagnosis of Gingivitis
The symptoms of gingivitis are relatively easy to recognize. They include red, swollen gums, bleeding during brushing or flossing, bad breath, and sometimes tender gums. These symptoms arise from the inflammation caused by bacterial plaque accumulating on the teeth and gums. In some cases, you might also notice receding gums or changes in the color of your gums, indicating the progression of the disease.
Diagnosing gingivitis typically involves a dental examination where the dentist will check for signs of inflammation, measure the depth of gum pockets, and assess the level of plaque and tartar on your teeth. During the examination, the dentist may use a small probe to measure the depth of the pockets around your teeth. Pockets deeper than 3 millimeters are often indicative of gum disease. The presence of bleeding, pus, or other signs of infection will also be noted. Early diagnosis is crucial to prevent the progression of gingivitis to more severe periodontal diseases, which can lead to tooth loss and other health complications.
Preventive Measures Against Gingivitis
Preventing gingivitis largely revolves around maintaining excellent oral hygiene. This includes brushing your teeth at least twice a day with fluoride toothpaste, flossing daily to remove plaque between your teeth, and using an antibacterial mouthwash to reduce the bacterial load in your mouth. Regular dental check-ups and professional cleanings are also essential.
- Brushing your teeth properly involves using a soft-bristled toothbrush and replacing it every three to four months. Ensure you brush for at least two minutes, covering all surfaces of your teeth and tongue. Flossing is equally important as removing food particles and plaque from areas your toothbrush cannot reach. Neglecting teeth brushing can lead to the rapid accumulation of plaque, resulting in gingivitis and other dental issues.
- An antibacterial mouthwash can help reduce the bacteria in your mouth, lowering the risk of plaque formation. Mouthwashes containing chlorhexidine or essential oils are particularly effective in controlling bacteria.
- Regular dental visits should be scheduled at least twice a year. During these visits, your dentist will perform professional cleanings to remove plaque and tartar that cannot be removed by regular brushing and flossing. These cleanings, known as scaling and polishing, are vital in maintaining gum health.
- In addition to these practices, a healthy diet low in sugar and nutrients can support gum health. Foods rich in vitamin C and calcium are particularly beneficial for maintaining strong teeth and gums.
- Avoiding tobacco products and limiting alcohol consumption can also significantly reduce your risk of developing gingivitis.
Treatment Strategies for Gingivitis
If you are diagnosed with gingivitis, your dentist will likely recommend a professional cleaning to remove all traces of plaque and tartar. This process, known as scaling and root planing, helps eliminate the bacterial colonies contributing to inflammation.
In addition to professional cleaning, your dentist may suggest using antiseptic mouthwashes and improved oral hygiene practices at home. In severe cases, additional treatments such as antibiotic therapy or even surgical interventions might be necessary. These comprehensive treatment strategies aim to reduce bacterial load, minimize inflammation, and restore the gums’ health, preventing gingivitis’s progression to more severe forms of periodontal disease.
Treatment Options:

- Scaling and Root planning is a deep-cleaning procedure that removes plaque and tartar from below the gum line and smooths the roots to prevent future bacterial colonization.
- Antiseptic Mouthwashes: Use chlorhexidine or other antiseptics to reduce bacterial load and inflammation in the gums.
- Improved Oral Hygiene Practices: Recommendations for brushing and flossing techniques, using interdental brushes, and regular dental check-ups to maintain oral health.
- Antibiotic Therapy: In cases where gingivitis does not respond to other treatments, antibiotics may be prescribed to control bacterial infection.
- Surgical Interventions: Procedures such as flap surgery or gingivectomy may be necessary to remove diseased gum tissue and reduce pocket depths around the teeth.
- Laser Therapy uses laser technology to remove inflamed gum tissue and tartar, promoting healing and reducing pocket depths.
- Diet and Lifestyle Changes: Advising patients to avoid smoking, reduce sugar intake, and maintain a diet rich in vitamins and minerals to support gum health.
Implementing these treatments can effectively manage and reverse gingivitis, ensuring long-term oral health and preventing further complications.
The Role of Oral Hygiene in Preventing Bad Breath
Maintaining good oral hygiene is paramount in preventing both gingivitis and bad breath. By brushing and flossing regularly, you can significantly reduce the bacterial load in your mouth, thereby minimizing the production of VSCs. Regular dental visits ensure that any early signs of gum disease are promptly addressed. Also, staying hydrated and avoiding foods contributing to bad breath can help maintain a fresh breath. Simple habits such as chewing sugar-free gum can also stimulate saliva production, which naturally cleanses the mouth and reduces bad breath.
Conclusion
In conclusion, while gingivitis is a mild form of gum disease, its impact on oral health, including its contribution to bad breath, should not be underestimated. You can prevent gingivitis through diligent oral hygiene practices and regular dental care and maintain a healthy, fresh-smelling mouth.

Dr. Orion Johnson is a dedicated and compassionate dentist committed to providing exceptional dental care to his patients.Dr. Johnson obtained his Doctor of Dental Surgery (DDS) degree from a prestigious dental school, where he excelled academically and clinically. He is licensed to practice dentistry and stays updated with the technology through continuing education and training.
