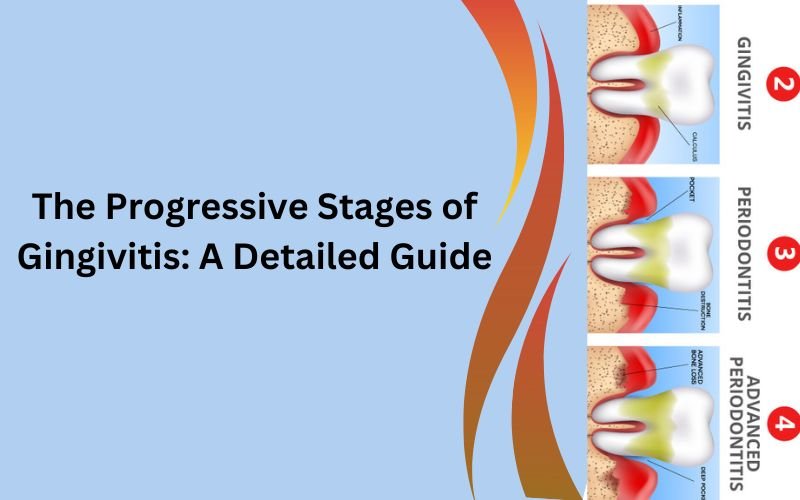
Gingivitis, an inflammation of the gums, is the preliminary stage of gum disease. It is often characterized by red, swollen gums that may bleed during brushing or flossing. This condition directly results from plaque buildup on the teeth, which can lead to more severe periodontal diseases if left untreated.
Gum disease, or periodontal disease, encompasses a range of conditions affecting the gums and supporting structures of the teeth. It begins with gingivitis and can progress to more severe stages if not addressed promptly. Understanding the progression of gum disease is crucial for effective prevention and treatment.
The Onset of Gingivitis: Stage 1
Gingivitis stage 1 is the initial phase of gum disease, marked by the accumulation of plaque on the teeth and gums. Plaque, a sticky film composed of bacteria, food particles, and saliva, adheres to the surfaces of the teeth, particularly along the gum line. If not removed through regular brushing and flossing, plaque hardens into tartar, which can only be removed by a dental professional.

At this early stage, the symptoms of gingivitis are often subtle. Slight redness and swelling of the gums are common, and the gums may bleed slightly when you brush or floss. This bleeding is one of the first signs that your gums need more attention. Despite these symptoms, there is usually no pain, which can make it easy to overlook the condition.
However, the beauty of gingivitis stage 1 is its reversibility. With diligent dental hygiene practices, including brushing at least twice a day with fluoride toothpaste, flossing daily to remove plaque between the teeth, and using an antiseptic mouthwash, the inflammation can be reduced and the gums can return to their healthy state. Regular visits to the dentist for professional cleanings are also essential in keeping plaque and tartar at bay.
Progression to Gum Disease: Stage 2
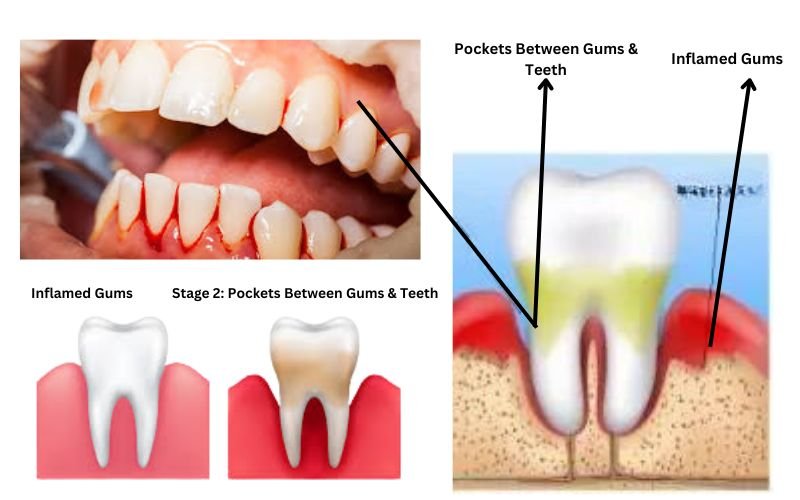
Gum disease stage 2, or early periodontitis, signifies a progression of gingivitis into the deeper tissues of the gums. This stage is marked by the development of pockets between the teeth and gums, where food particles, bacteria, and plaque accumulate. These pockets create an environment where bacteria thrive, exacerbating the inflammation and infection.
As the disease progresses, the gums may start to recede, exposing the roots of the teeth. This can lead to increased sensitivity to hot and cold temperatures, making eating and drinking uncomfortable. The presence of these pockets can also result in chronic bad breath and a foul taste in the mouth, further indicating the presence of infection.https://photobloge.com/teeth/teeth-infection/
At this stage, more intensive cleaning is required. Scaling and root planing, a deep cleaning procedure performed by a dentist or periodontist, is often necessary to remove tartar from above and below the gum line and to smooth the root surfaces, making it more difficult for bacteria to adhere. In addition to professional cleanings, improving at-home oral care practices is crucial to prevent further progression.
Advanced Gum Disease: Level 3
Gum disease level 3, or advanced periodontitis, represents the most severe form of gum disease. At this stage, the infection has caused significant damage to the supporting structures of the teeth, including the periodontal ligament and alveolar bone. This destruction can result in loose teeth, shifting of the bite, and even tooth loss.
The symptoms of advanced periodontitis are more pronounced and can include swollen, pus-filled gums, severe bad breath, and significant gum recession. The damage to the bone and connective tissue is often irreversible, making the management of the disease more complex.

Treatment for advanced gum disease typically involves surgical interventions to restore gum and bone health. Procedures such as flap surgery, bone grafts, and soft tissue grafts may be necessary to repair the damage caused by the disease. In addition, ongoing maintenance therapy, including frequent professional cleanings and diligent at-home care, is essential to manage the condition and prevent further deterioration.
Recognizing Symptoms of Gingivitis
Identifying the symptoms of gingivitis early can prevent the condition from progressing to more severe stages.
- Common signs include persistent bad breath, tender gums, bleeding during brushing or flossing, and a noticeable change in gum color from pink to red.
- Other symptoms might include swollen gums, discomfort while chewing, and a receding gum line. These early warning signs should prompt immediate attention to oral hygiene and a visit to the dentist.
Recognizing these symptoms can help in taking timely action to reverse the condition and prevent further complications.
Common Causes of Gingivitis
Several factors contribute to the development of gingivitis.
- Poor oral hygiene is the primary cause, allowing plaque to build up on teeth and gums. Smoking significantly increases the risk, as it weakens the immune system and hampers gum healing.
- Hormonal changes during puberty, menstruation, pregnancy, and menopause can also make gums more sensitive to gingivitis.
- Certain medications that reduce saliva flow can lead to dry mouth, increasing the risk of gum disease.
- Underlying health conditions like diabetes can impair the body’s ability to fight infections, including those in the mouth.
Understanding these causes is crucial for implementing effective preventive measures.
The Impact of Braces on Gingivitis
Gingivitis from braces is a common issue due to the difficulty in maintaining oral hygiene with orthodontic appliances. Braces can trap food particles and plaque, leading to increased gum inflammation. The brackets and wires of braces create numerous nooks and crannies where plaque and food particles can accumulate, making it challenging to keep the teeth and gums clean.
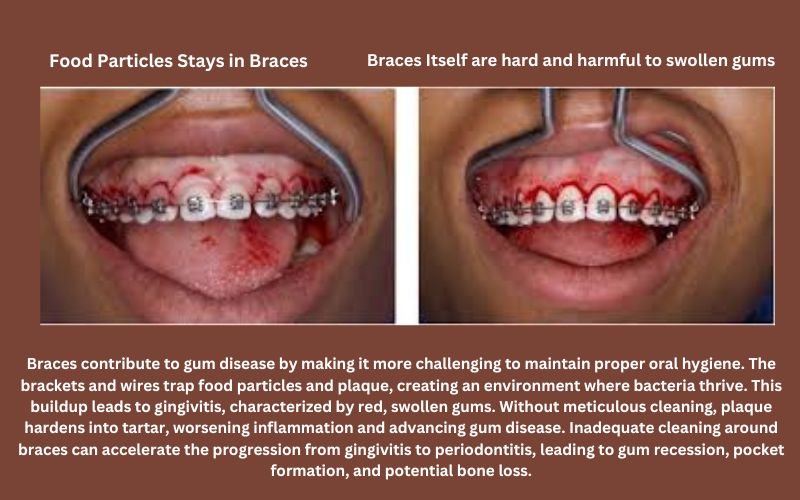
Special care and dental tools are necessary to manage gum health for individuals with braces. Using an interdental brush or a proxabrush can help clean between the brackets and under the wires, reaching areas that a regular toothbrush might miss. Water flossers are also highly effective in dislodging food particles and plaque from around the braces.
Adopting a meticulous oral hygiene routine is essential for those with braces. This includes brushing after every meal, using fluoride toothpaste, and rinsing with an antiseptic mouthwash to reduce bacterial growth. Maintaining this routine can significantly reduce the risk of developing gingivitis and ensure that the teeth and gums remain healthy throughout the orthodontic treatment.
The Role of Vitamins in Gum Health
Gum disease vitamins play a crucial role in maintaining healthy gums.
- Vitamin C, for instance, is essential for collagen production and repairing connective tissues. A deficiency in this vitamin can lead to weakened gums and increased susceptibility to gingivitis. Vitamin C also acts as an antioxidant, combating the damaging effects of free radicals on gum tissues.
- Vitamin D is another important nutrient, playing a key role in calcium absorption and bone health, which supports the underlying structures of the teeth. A deficiency in Vitamin D can lead to bone loss and compromise the integrity of the teeth and gums.
- B-complex vitamins, including B12 and folic acid, are vital for maintaining the overall health of the oral mucosa and reducing gum inflammation.
These vitamins support cell regeneration and enhance the body’s immune response, helping to ward off infections that can lead to gum disease. Ensuring an adequate intake of these essential vitamins through diet or supplements can significantly enhance gum health and prevent the onset of gum diseases like gingivitis.
Treatment Options for Gingivitis
Treating gingivitis involves professional dental care and improved personal oral hygiene.
- Professional treatments may include deep cleaning procedures like scaling and root planing, which remove plaque and tartar from below the gum line and smooth the root surfaces, making it harder for bacteria to adhere. These procedures are often complemented by the use of antibacterial agents to control the infection.
- At home, maintaining a rigorous oral hygiene routine is crucial. This includes brushing twice daily with antibacterial toothpaste, flossing to remove food particles and plaque between teeth, and rinsing with an antiseptic mouthwash to reduce bacterial load.
- In severe cases, where gingivitis has progressed to more advanced forms of gum disease, antibiotics may be prescribed to combat the infection. Surgical interventions, such as flap surgery or bone and tissue grafts, may also be necessary to repair and regenerate damaged tissues.
Early and consistent treatment is key to reversing gingivitis and preventing its progression to more severe periodontal diseases.
Conclusion
Understanding the stages of gingivitis is crucial for effective prevention and treatment. From recognizing early symptoms and the impact of braces to the role of vitamins and the importance of regular dental check-ups, proactive oral care can prevent the progression of gum disease. Maintaining good oral hygiene and seeking timely professional care are essential steps to ensure healthy gums and overall oral health.

Dr. Orion Johnson is a dedicated and compassionate dentist committed to providing exceptional dental care to his patients.Dr. Johnson obtained his Doctor of Dental Surgery (DDS) degree from a prestigious dental school, where he excelled academically and clinically. He is licensed to practice dentistry and stays updated with the technology through continuing education and training.