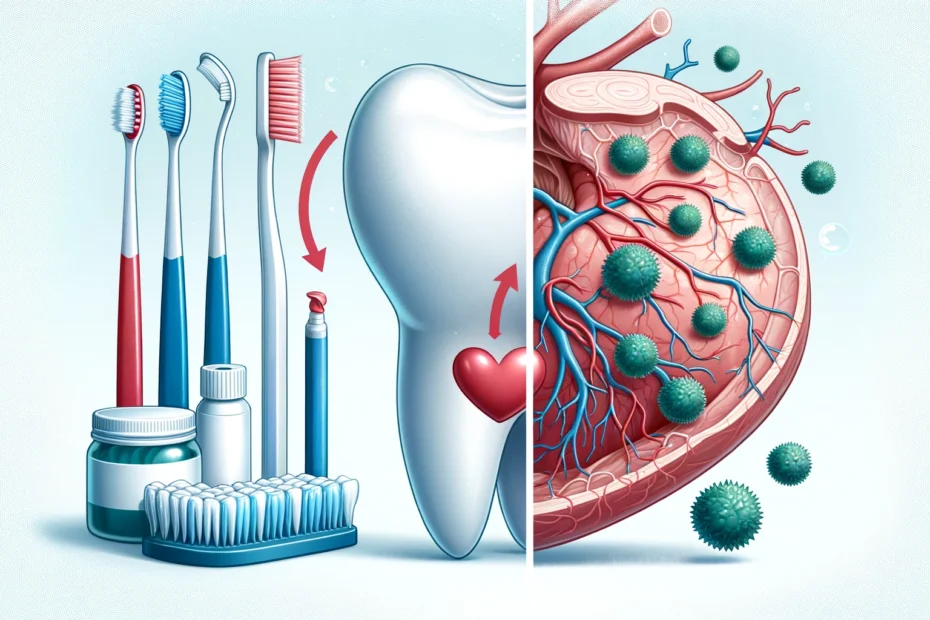
Oral hygiene, often overlooked in the grand scheme of health, plays a pivotal role far beyond the confines of our mouths. There’s a compelling connection between oral health and heart disease; the state of our gums and teeth can significantly influence our cardiovascular well-being. Understanding this relationship is crucial in fostering both oral and overall health.
Oral hygiene refers to practices that keep our mouths clean and disease-free. This includes regular brushing, flossing, and dental check-ups. Proper oral hygiene prevents common dental problems like cavities, gingivitis, and periodontitis. If left unchecked, these conditions can lead to more severe health issues, underscoring the importance of diligent oral care.
The Connection Between Oral Health and Heart Disease
The link between oral health and heart disease might seem tenuous at first glance, but a growing body of research supports this association.
Poor oral hygiene can lead to periodontal disease, a severe gum infection that can spread bacteria and cause inflammation. These bacteria and inflammatory markers have been found in the arterial plaques of those suffering from atherosclerosis, a major risk factor for heart disease.
When oral hygiene is neglected, dental plaque builds up, leading to gingivitis and periodontitis. Gingivitis, the initial stage of gum disease, is characterized by redness, swelling, and bleeding gums. If untreated, it progresses to periodontitis, where the gums pull away from the teeth, forming pockets that become infected. The body’s immune response to this infection can be intense, releasing substances that break down bone and connective tissue, eventually leading to tooth loss.
This inflammatory process is not confined to the mouth. The bacteria and inflammatory markers from periodontal disease can enter the bloodstream, traveling to other body parts, including the heart. These bacteria contribute to forming and exacerbating atherosclerotic plaques in the arteries. Atherosclerosis, the buildup of fatty deposits in the arterial walls, is a significant risk factor for heart disease, leading to conditions such as coronary artery disease, angina, and heart attacks.
Individuals with periodontal disease are nearly twice as likely to suffer from heart disease as those with healthy gums. The severity of the gum disease correlates with the risk of cardiovascular problems, suggesting a dose-response relationship.
The Role of Bacteria in Oral and Cardiovascular Health
Bacteria are omnipresent in our mouths, with over 700 species residing in the oral cavity. While many are harmless, some can cause significant harm if oral hygiene is neglected. Pathogenic bacteria can enter the bloodstream through inflamed gums, leading to systemic infections. These bacteria can adhere to the arterial walls, contributing to the formation of atherosclerotic plaques, thus impairing cardiovascular health.
The mouth serves as a gateway to the body, and pathogenic oral bacteria can easily breach the barriers when gum disease is present. For instance, Porphyromonas gingivalis, Tannerella forsythia, and Treponema denticola are commonly implicated in periodontitis and have been found in arterial plaques. These bacteria can evade the immune system and induce a robust inflammatory response, exacerbating cardiovascular conditions.
Once in the bloodstream, these bacteria can contribute to the development of endocarditis, an infection of the inner lining of the heart chambers and valves. Endocarditis can occur when bacteria from the mouth enter the bloodstream and attach to damaged areas of the heart. This infection is particularly dangerous for individuals with pre-existing heart conditions, as it can lead to severe complications, including heart failure.
Additionally, the endotoxins produced by these bacteria can directly damage the endothelium, the inner lining of blood vessels. This damage can lead to increased permeability and the development of atherosclerotic lesions. The body’s immune response to these endotoxins further contributes to the inflammatory process, promoting the growth and instability of plaques. These unstable plaques are more likely to rupture, causing blood clots that can block arteries and lead to heart attacks or strokes.
Inflammation: The Silent Culprit
Inflammation is a critical link between oral health and heart disease. Chronic inflammation in the mouth, often due to gum disease, can lead to systemic inflammation. This persistent inflammatory response can damage blood vessels, facilitate plaque build-up in arteries, and ultimately increase the risk of heart attacks and strokes. Addressing oral inflammation is, therefore, crucial in mitigating cardiovascular risks.
- When the gums are inflamed, they release pro-inflammatory cytokines, such as interleukin-1 (IL-1), interleukin-6 (IL-6), and tumor necrosis factor-alpha (TNF-alpha). These cytokines can enter the bloodstream and contribute to systemic inflammation. Elevated levels of these inflammatory markers are commonly found in individuals with cardiovascular disease, suggesting a link between periodontal inflammation and heart disease.
- Systemic inflammation can exacerbate the development of atherosclerosis by promoting the recruitment of inflammatory cells to the arterial walls. These cells, including macrophages and T-lymphocytes, contribute to forming fatty streaks, the earliest visible lesions of atherosclerosis. Over time, these fatty streaks develop into more advanced plaques, obstructing blood flow and increasing the risk of cardiovascular events.
- Moreover, chronic inflammation can induce oxidative stress, a condition characterized by an imbalance between the production of free radicals and the body’s ability to neutralize them. Oxidative stress can further damage the endothelium and promote low-density lipoprotein (LDL) cholesterol oxidation, a key step in forming atherosclerotic plaques. Oxidized LDL within the plaques makes them more prone to rupture, posing a significant threat to cardiovascular health.
Gum disease, particularly periodontitis, has a profound impact on heart health. This advanced form of gum disease destroys the tissues supporting the teeth and serves as a gateway for bacteria to enter the bloodstream.
Preventative Measures for Optimal Oral and Heart Health
Maintaining optimal oral and heart health requires a proactive approach.
Regular Dental Visits:
Regular dental visits are crucial for maintaining both oral and heart health.
- Schedule biannual dental check-ups.
- Professional cleanings remove plaque and tartar.
- Early detection of gum disease and other oral issues.
Proper Brushing Techniques:
Proper brushing techniques help prevent oral health issues that can impact heart health. Neglecting brushing properly can lead to different problems.
- Brush at least twice a day with fluoride toothpaste.
- Use a soft-bristled toothbrush to prevent gum damage.
- Replace the toothbrush every three months or sooner if the bristles are frayed.
Effective Flossing:
Effective flossing is essential for removing plaque and preventing gum disease.
- Floss daily to remove plaque and food particles between teeth.
- Use dental floss or interdental cleaners.
- Proper technique involves gently sliding the floss between the teeth and below the gumline.
Balanced Diet:
A balanced diet supports both oral and cardiovascular health.
- Consume a diet rich in fruits, vegetables, whole grains, and lean proteins.
- Limit sugar and acidic foods to prevent tooth decay.
- Ensure adequate intake of oral hygiene vitamins and minerals, especially calcium and vitamin D.
Manage Chronic Conditions:
Managing chronic conditions like diabetes is crucial for reducing oral and heart disease risks.
- Control diabetes through medication, diet, and exercise.
- Monitor blood sugar levels to reduce the risk of gum disease.
- Regularly check for signs of gum disease if diabetic.
Patient Education:
Educating patients about oral health is essential for preventing heart disease.
- Stay informed about the importance of oral hygiene.
- Educate family and friends on the connection between oral and heart health.
- Use reputable sources for information on maintaining oral health.
Treatments for Gum Disease and Heart Health
Treatments for gum disease and heart health are integral to overall well-being.
- Scaling and Root Planing: Scaling and root planing is a deep cleaning procedure designed to remove plaque and tartar below the gum line. This treatment smooths the roots of teeth, helping the gums reattach and heal more effectively.
- Antibiotic Therapy: Antibiotic therapy, involving topical or oral antibiotics, is often used with scaling and root planing to eliminate bacterial infections. This approach helps reduce inflammation and bacterial load, facilitating the healing process. Antibiotics target the bacteria responsible for gum disease, providing a comprehensive treatment strategy.
- Surgical Treatments: Surgical treatments for gum disease include various procedures such as flap surgery, bone and tissue grafts, and guided tissue regeneration. Flap surgery involves lifting the gums to remove tartar deposits and then suturing them back into place.
- Medications for Heart Health: Heart-health medications are crucial in managing the cardiovascular risks associated with poor oral health. Statins are commonly prescribed to lower cholesterol and reduce plaque formation within the arteries.
Conclusion
The intricate relationship between oral hygiene and heart disease highlights the importance of a holistic approach to health. By understanding and addressing the factors that link our oral health to our cardiovascular system, we can adopt practices that benefit our overall well-being. Prioritizing oral hygiene is not merely about preserving a bright smile; it is critical to sustaining a healthy heart and a vibrant life.

Dr. Orion Johnson is a dedicated and compassionate dentist committed to providing exceptional dental care to his patients.Dr. Johnson obtained his Doctor of Dental Surgery (DDS) degree from a prestigious dental school, where he excelled academically and clinically. He is licensed to practice dentistry and stays updated with the technology through continuing education and training.