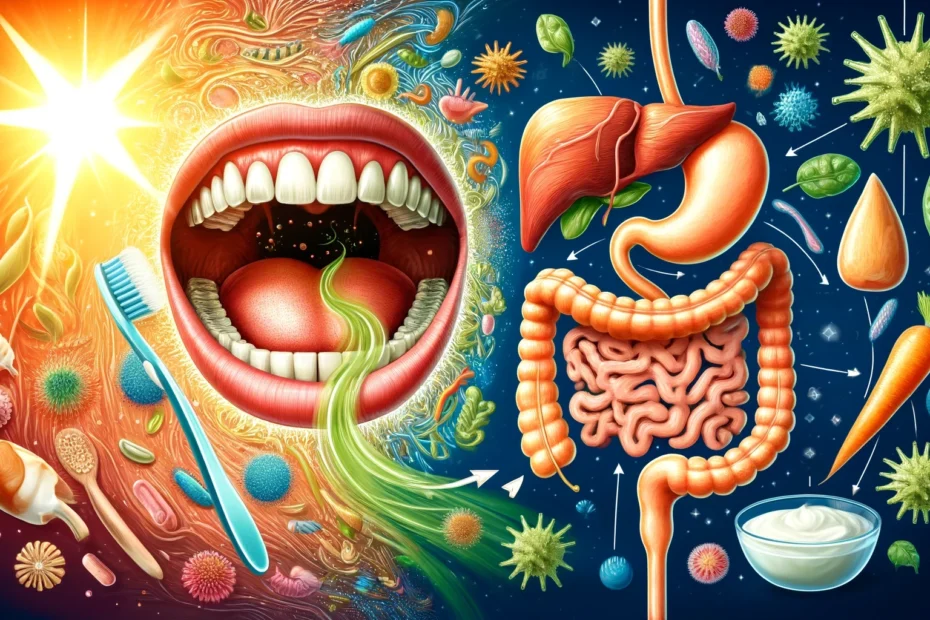
Oral health and gut bacteria are intricately linked, significantly impacting our overall well-being. Understanding this relationship can lead to better health outcomes and innovative treatments.
This article explores the connection between the oral microbiome and gut bacteria, shedding light on how one affects the other and what can be done to maintain a healthy balance.
Understanding the Oral Microbiome
The oral microbiome consists of a complex community of microorganisms in the mouth, including bacteria, fungi, viruses, and protozoa. These microbes form biofilms, such as dental plaque, which play crucial roles in oral health and disease.
A balanced oral microbiome helps in the initial digestion of food, protection against pathogens, and maintaining the integrity of oral tissues. Disruptions in this balance can lead to cavities, periodontal disease, and systemic infections.
The Gut Microbiome: An Overview
The gut microbiome is an extensive ecosystem of microorganisms inhabiting the gastrointestinal tract. It includes trillions of bacteria, viruses, fungi, and other microbes. These organisms are essential for various bodily functions, including digestion, immune system modulation, and the production of vitamins and other bioactive compounds.
A diverse and stable microbial population characterizes a healthy gut microbiome. Dysbiosis, or an imbalance in the gut microbiome, has been linked to numerous health issues, such as inflammatory bowel disease, obesity, and mental health disorders.
The Oral-Gut Axis: How Are They Connected?
The oral gut axis refers to the bidirectional relationship between the microorganisms in the mouth and those in the gut. This connection is facilitated by the continuous flow of saliva and swallowed microorganisms, which travel from the oral cavity to the gastrointestinal tract. This movement can introduce oral bacteria to the gut, influencing its microbial composition.
Conversely, systemic conditions affecting the gut can also impact oral health. Understanding this axis is crucial for comprehending the broader implications of oral and gut microbiome interactions on general health.
- For example, research has shown that certain oral pathogens, such as Porphyromonas gingivalis, can influence the gut microbiome’s composition and exacerbate inflammatory bowel disease (IBD).
- Similarly, matters gut-related as irritable bowel syndrome (IBS) can be reflected in oral health problems, underscoring the interconnectedness of these two microbiomes.
The oral-gut axis also highlights the importance of holistic health approaches. Treatments that target one microbiome can inadvertently affect the other, suggesting that healthcare providers should consider the state of both the oral and gut microbiomes when diagnosing and treating diseases.
For instance, probiotics commonly used to support gut health may also benefit oral health by reducing inflammation and promoting beneficial bacteria in the mouth.
How Gut Health Affects Oral Health
Just as oral health impacts the gut, gut health reciprocally influences oral health. A disrupted gut microbiome can lead to systemic inflammation, manifesting as periodontal disease or other inflammatory conditions in the oral cavity.
- Nutrient absorption issues due to poor gut health can also affect oral tissues, making them more susceptible to infections and other problems.
- Probiotics and prebiotics that promote a healthy gut microbiome can indirectly support oral health by reducing systemic inflammation and improving nutrient status.
Common Oral Health Issues Linked to Gut Dysbiosis
Several oral health issues are linked to gut dysbiosis. For example, periodontal disease has been associated with inflammatory bowel disease, suggesting a shared inflammatory pathway. Bad breath, or halitosis, can sometimes be traced back to gut imbalances.
Periodontal Disease:
A chronic condition affecting the gums and supporting structures of the teeth, often linked to systemic inflammation.
- Linked to inflammatory bowel disease (IBD), indicating a shared inflammatory mechanism.
- Chronic inflammation in the gut can exacerbate periodontal conditions, leading to severe gum disease.
- Oral pathogens can migrate to the gut, aggravating existing gastrointestinal issues.
Halitosis (Bad Breath):
Persistent bad breath can signal deeper health issues, often stemming from an imbalance in the gut microbiome.
- Often a result of an imbalanced gut microbiome.
- Certain gut bacteria produce volatile sulfur compounds, contributing to foul breath.
- Poor digestion and gut dysbiosis can lead to accumulation these compounds in the mouth.
Oral Thrush
This fungal infection, characterized by white patches in the mouth, can frequently be traced back to compromised gut health.
- Fungal infections, such as Candida overgrowth, are more common in individuals with gut dysbiosis.
- A compromised gut microbiome can reduce the body’s ability to fight off fungal infections in the mouth.
- Recurrent oral thrush can be a sign of underlying gut health issues.
Dental Caries (Cavities):
Cavities are a common oral health issue that dietary habits and gut microbiome health can influence.
- A diet high in sugar and refined carbohydrates can promote the growth of harmful bacteria in both the mouth and gut.
- Gut dysbiosis can lead to nutrient absorption issues, weakening tooth enamel, and increasing susceptibility to cavities.
Gingivitis:
Inflammation of the gums can serve as an early warning sign of more serious oral and systemic health problems.
- Mild inflammation of the gums that can be exacerbated by gut dysbiosis.
- Poor gut health can lead to systemic inflammation, affecting the gums and oral tissues.
- Addressing gut health can help in reducing the severity of gingivitis.
Strategies for Maintaining a Healthy Oral-Gut Microbiome Balance
Maintaining oral hygiene is essential for a healthy oral gut microbiome balance.
- Brush teeth at least twice daily with fluoride toothpaste to remove plaque and prevent tooth decay. Avoiding brushing twice a day can lead to serious problems.
- Floss daily to remove food particles and plaque between teeth and along the gumline.
- Regular dental check-ups and cleanings to monitor and maintain oral health.
In addition to good oral hygiene practices, dietary choices play a significant role in supporting beneficial bacteria.
- Consume a diet rich in fiber from fruits, vegetables, and whole grains to support beneficial bacteria.
- Incorporate fermented foods like yogurt, kefir, sauerkraut, and kimchi to introduce probiotics.
- Limit refined sugars and processed foods intake, which can promote harmful bacterial growth.
Additionally, oral thrush, a fungal infection, can occur more frequently in individuals with compromised gut health. Recognizing these connections can lead to more holistic approaches to diagnosing and treating oral health issues.
Conclusion
The connection between oral health and gut bacteria is a fascinating and complex relationship that underscores the importance of maintaining good hygiene and a balanced diet. By understanding and nurturing the oral-gut axis, we can improve our oral and digestive health and overall well-being. As research continues to unravel the mysteries of the microbiome, the potential for novel therapeutic strategies and improved health outcomes becomes ever more promising.

Dr. Orion Johnson is a dedicated and compassionate dentist committed to providing exceptional dental care to his patients.Dr. Johnson obtained his Doctor of Dental Surgery (DDS) degree from a prestigious dental school, where he excelled academically and clinically. He is licensed to practice dentistry and stays updated with the technology through continuing education and training.